You’re reading Third Horizon’s 2025 monthly blog series on health care innovation and resilience. Throughout the year, we will bring our unique perspective to bear across our three advisory areas: Behavioral Health, Community Health, and Payment Design and Analytics.
This month’s focus: The impact of policy turbulence on longstanding public health efforts.
Listen to the article
By Tym Rourke, MA, Managing Director for Community Health, Erica Bauer, PhD, Director, and Topher Rasmussen, MSW, Communications Manager
The Trump administration has made “Making America Healthy Again” a cornerstone of its health policy agenda, with particular emphasis on addressing the nation’s chronic disease burden. There is compelling reason to focus in this area—chronic diseases account for seven of the top 10 causes of death in the United States and consume over 80 percent of health care dollars. However, while the rhetoric emphasizes chronic disease reduction, recent policy, fiscal and regulatory decisions may exacerbate these conditions.
The Trump administration is seeking to cut approximately one-third in discretionary spending by the Department of Health and Human Services (HHS), which would reduce the HHS budget from about $121 billion to $80 billion. Separately, the administration has already clawed back $11.4 billion in pandemic-related health funding, prompting New York, along with 22 other states and Washington DC, to file a lawsuit. These terminated funds, originally provided during the COVID-19 pandemic, were being used by states to address gaps in public health infrastructure, behavioral health, and other health-related social needs. Additionally, Centers for Disease Control and Prevention (CDC) and National Institute of Health (NIH) grant terminations have slowed or halted scientific research, much of which is tied to chronic disease monitoring and treatment.
The Nation’s Public Health Infrastructure Compromised
In addition to funding cuts, the administration has removed over 20,000 employees from HHS – via terminations or incentivized retirement programs – and begun a massive restructuring effort within the department. Entire divisions or units focusing on specific public health threats have been eliminated. For example, the Substance Use and Mental Health Services Administration (SAMHSA) and others are being directed to fold into a single “Administration for a Healthy America.”
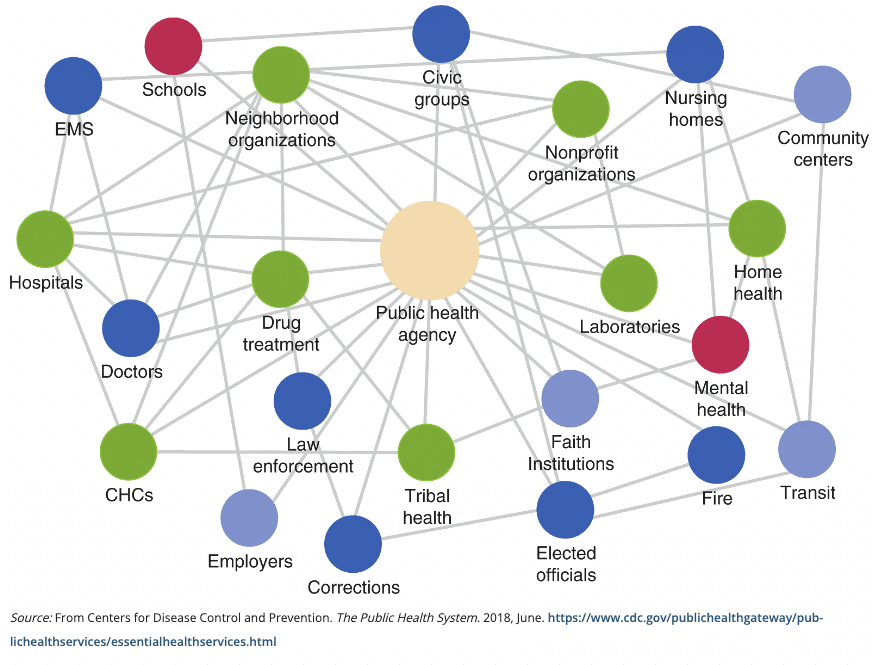
Primary prevention—stopping chronic disease before it develops—requires robust public health infrastructure, seamless communication across systems, reliable data, and sustained financing. However, current administration policy and regulatory directions suggest a shift away from established prevention frameworks toward a more reactionary approach, with a decrease in real time data and communications to prepare and support communities, and a renewed focus on root causes of chronic disease that, in some instances, have been disproven in established science. These actions risk creating gaps in our chronic disease prevention ecosystem.
The current approach also seems to minimize the social drivers of health—factors like economic stability, education, and neighborhood conditions that significantly influence chronic disease risk – and restrict critical data and analysis necessary to ensure that public health approaches and interventions are accessible to all Americans. Addressing these upstream factors requires cross-sector collaboration and sustained investment, both of which appear diminished in current federal priorities.
Though specifics about HHS reorganizing steps remain unclear, Community Based Organizations (CBOs) that rely on funding, data, and technical assistance from these agencies, have voiced concerns that consolidation efforts may reduce focus, attention, and capacity to address significant public health and chronic disease efforts in local communities.
For health care organizations navigating this landscape, the message is mixed. The commitment to addressing chronic disease suggests potential partnerships and initiatives, yet the funding reductions and agency restructuring signal different priorities. The disconnects between stated goals and policy implementation create substantial inefficiencies. Health care organizations must now develop parallel strategies—one aligned with the stated chronic disease priorities and another accounting for the reality of reduced resources and federal support. This dual planning process consumes valuable organizational bandwidth and diverts attention from patient care.
A Path Forward: Strategic Recommendations
For health care and social service organizations navigating this complex environment, several approaches may help maintain focus on chronic disease reduction despite policy and fiscal headwinds, while positioning systems for more resiliency as the impacts of changes in federal policy continue to take shape:
Expand the use of local data to track and monitor chronic disease risk and prevalence. Early in the new administration, several key public health data sets were removed from federal websites, including the Social Vulnerability Index (SVI) and the Youth Risk Behavior Survey (YRBS). Though many of these data sets were returned to federal sites, there remains a lack of clarity around federal interest or capacity to continue collecting and publishing these critical data sets. CBOs should begin to augment their use of these data sets with locally collected data, to ensure an ongoing ability to track chronic disease and its impacts. This may entail researching other existing data tools, or establishing new data agreements with aligned groups to ensure gaps caused by potential losses of federal data collection capacity are avoided where possible. A continued effort to collect data not only can assist in informing local strategy, but can help policymakers and the local, regional, state and national level understand the practical implications of funding decisions.
Take time to strengthen and foster cross-sector partnerships. Develop collaborations with community organizations, educational institutions, and private sector entities to address chronic disease drivers outside traditional healthcare settings. These partnerships can help mitigate the impact of reduced federal support and unlock potential opportunities to leverage partnerships to sustain and grow a community’s public health response.
Focus on efficiency in service delivery. Implement care delivery models and community strategies that maximize efficiency without compromising quality. Better leverage of telehealth, shared data systems, and natural community channels in communities can protect the ability to deliver care, enhance partnerships, and provide critical messaging to the community on actions it can take to limit and reduce the prevalence and burden of chronic disease.
Integrate “resiliency” into organizational planning efforts. CBOs often focus on sustainability when developing or adjusting strategic or business plans. However, sustainability is often treated as an “end game” – when it should be considered an ongoing part of strategic development. Organizational leaders, nonprofit boards, and community health coalitions should begin to reframe the conversation around resiliency. The current climate brings unanticipated concerns and potential threats. While in many respects this moment feels unprecedented, periods of fiscal and regulatory stability are often disrupted by factors beyond an organization’s control (a sudden pandemic, an economic downturn, etc.). Organizations should be exploring how institutions, community partnerships, and systems can adapt and navigate through uncertain times. Disruption is inevitable; organizations best suited for managing these disruptions are those that spend time preparing. As tumultuous as this moment is, it brings an opportunity to think through sustainability and resiliency of our public health and social service system, differently.
Drive workforce adaptation, retention and recruitment at the local level: Work to expand both internal and community-based training programs that enhance the ability of primary care providers, community health workers, and social service agency staff to support those with complex chronic conditions when specialty access is limited. This “up-training” approach can help bridge gaps in the care continuum.
Deepen organizational communication on policy choices that impact public health and chronic disease mitigation. Maintain active dialogue with policymakers at the local, regional, state, and national levels, providing frontline perspectives on how funding decisions impact chronic disease outcomes. This engagement should be evidence-based and non-partisan, as well as focused on population health impacts rather than political positioning. When possible, encourage those who are impacted by your work to speak up to ensure the stories of impact are centered in the lived experience of those who may benefit or be harmed by changes in policy.
Conclusion: Steadying the Ship
The current disconnect between chronic disease rhetoric and policy implementation presents significant challenges for health care organizations and the communities they serve. However, by acknowledging this gap and developing strategic responses, the health and social service sector can help mitigate negative impacts while continuing to advocate for evidence-informed policy approaches that reliably achieve positive public health outcomes. By focusing in this way, health care and social safety net leaders can help create a more coherent national approach to chronic disease—one where resources align with messaging and all Americans have access to the care they need to prevent, manage, and overcome chronic conditions.
At Third Horizon, we stand ready to work with community leaders, CBOs, and public entities that are working to navigate these complex policy environments, while maintaining focus on population health despite shifting priorities and resource constraints. As providers navigate these moments, and local communities and collaborations come together to chart a course responsive to the moment, we welcome opportunities to learn how we might be able to support organizations and communities in deepening our collective ability to reduce the burden caused by chronic disease and improve community health.